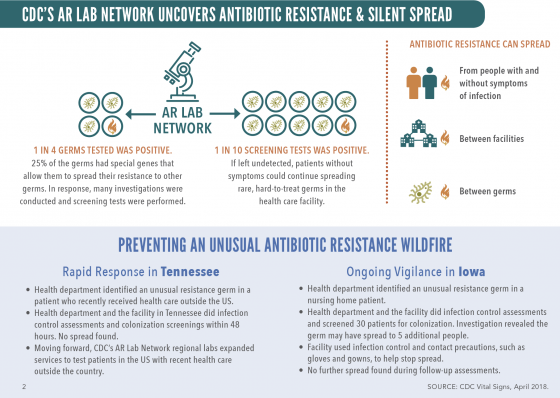
New nationwide testing in 2017 uncovered 221 instances of unusual resistance genes in what is known as “nightmare bacteria,” according to the Center for Disease Control and Prevention’s (CDC) monthly Vital Signs report, released last week. Germs with unusual antibiotic resistance (AR) include those that cannot be killed by all or most antibiotics, are uncommon in a geographic area or the U.
S., or have specific genes that allow them to spread their resistance to other germs.
Examples of AR germs include: Vancomycin-resistant Staphylococcus aureus (VRSA), Candida auris, and certain types of nightmare bacteria such as carbapenem-resistant Enterobacteriaceae (CRE).
“CDC’s study found several dangerous pathogens, hiding in plain sight, that can cause infections that are difficult or impossible to treat,” said CDC Principal Deputy Director Anne Schuchat, M.D.
With spring break in full effect and peak travel season on the horizon, the timing of this new information should be noted by businesses and the public, since AR has been found in every state and can spread between facilities and even people without symptoms of infection.
The CDC warned that germs “will continuously find ways to resist new and existing antibiotics” and that it is currently impossible to stop new resistances from developing. Recent nationwide infrastructure investments in laboratories, infection control, and response are enabling aggressive investigations to keep resistance from spreading in health care settings.
According to the CDC, a hard-to-treat germ that spreads easily was found in 11% of screening tests among subjects who displayed no symptoms. The nightmare germs sicken 2 million Americans and kill 23,000 every year. Additional study findings showed that:
- One-in-four germ samples sent to the AR Lab Network for testing had special genes that allow them to spread their resistance to other germs.
- Further investigation in facilities with unusual resistance revealed that about one in 10 screening tests, from patients without symptoms, identified a hard-to-treat germ that spreads easily.
buy flexeril online www.handrehab.us/images/patterns/jpg/flexeril.html no prescription pharmacy
This means the germ could have spread undetected in that health care facility.
buy anafranil online www.handrehab.us/images/patterns/jpg/anafranil.html no prescription pharmacy - For CRE alone, estimates show that the containment strategy would prevent as many as 1,600 new infections in three years in a single state—a 76% reduction.
The CDC’s rapid response Containment Strategy is launched at the first sign of unusual resistance. Recent cases were found and isolated in Tennessee, after a patient received health care outside the U.S.; and in Iowa, when a nursing home patient was diagnosed with an AR germ that spread to five other people. Follow-up assessments revealed the outbreak had been contained.
To mitigate the risk of contracting these germs, employees should:
- Inform your healthcare provider if you recently received health care in another country or facility.
- Talk to your healthcare provider about preventing infections, taking good care of chronic conditions and getting recommended vaccines.
CDC recommends practicing good hygiene, such as keeping hands clean with hand washing or alcohol-based hand rubs, and keeping cuts clean until healed.

 Hazardous work zones continue to affect the careers and companies of employees in the U.
Hazardous work zones continue to affect the careers and companies of employees in the U.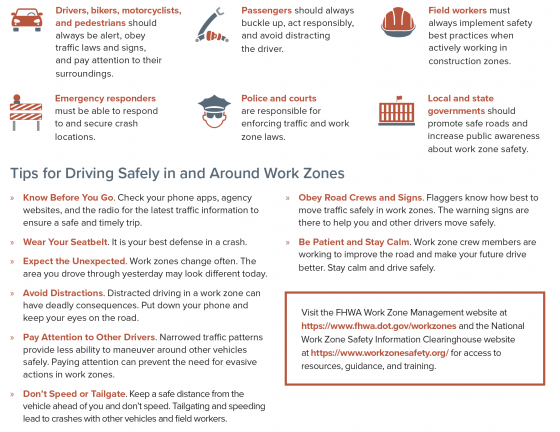
 With the northeast hammered by its fourth major snowstorm this month, businesses and property owners in many areas are digging out, breaking out the salt pellets and shovels (just when they were hoping to stash them for the next eight months).
With the northeast hammered by its fourth major snowstorm this month, businesses and property owners in many areas are digging out, breaking out the salt pellets and shovels (just when they were hoping to stash them for the next eight months).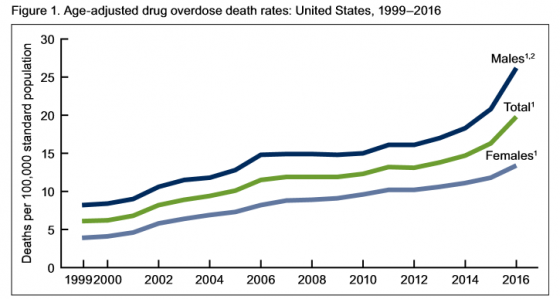
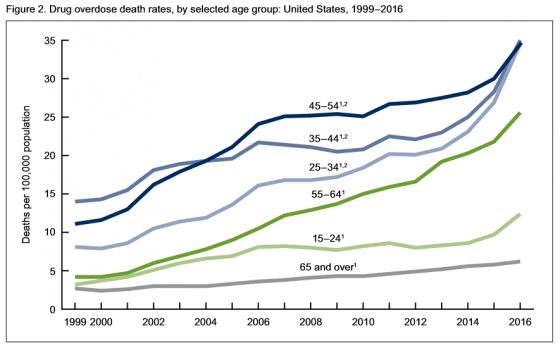
Authors of the report noted, “The pattern of drugs involved in drug overdose deaths has changed in recent years. The rate of drug overdose deaths involving synthetic opioids other than methadone (drugs such as fentanyl, fentanyl analogs, and tramadol) doubled in a single year from 3.1 per 100,000 in 2015 to 6.2 in 2016. Additionally, it’s important to note that many drug overdose deaths may involve multiple drugs.”
Of people age 15 and above:
• Rates of drug overdose deaths increased from 1999 to 2016 for all groups studied.
• Rates in 2016 were highest for people between the ages of 25 and 54.
• From 2015 to 2016, the drug overdose death rates for adults age 45-54, 55-64 and 65 and above went up 15%, 17% and 7% respectively, the CDC said.
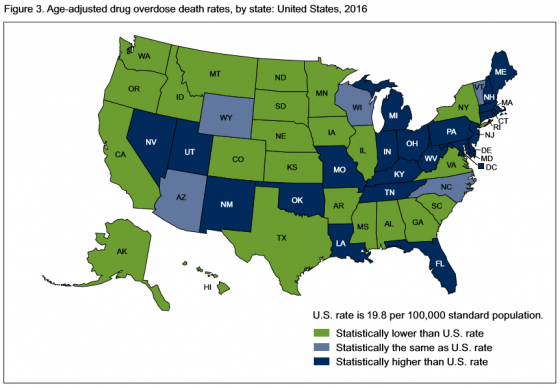
 In 2016, 22 states and the District of Columbia had overdose death rates that were statistically higher than the national rate. States with the highest number of overdose deaths were: West Virginia, with 52 per 100,000; Ohio with 39.1; New Hampshire with 39; District of Columbia with 38.8; and Pennsylvania, which had 37.9 deaths per 100,000.
In 2016, 22 states and the District of Columbia had overdose death rates that were statistically higher than the national rate. States with the highest number of overdose deaths were: West Virginia, with 52 per 100,000; Ohio with 39.1; New Hampshire with 39; District of Columbia with 38.8; and Pennsylvania, which had 37.9 deaths per 100,000.
States with the lowest age-adjusted drug overdose rates were: Iowa, which had 10.6 deaths; North Dakota, 10.6; Texas, 10; South Dakota, 8.4; and Nebraska, which had 6.4 deaths.
 In it’s most recent study, Quest Diagnostics found that workforce use of illicit drugs across the board—including cocaine, marijuana and methamphetamine—has climbed to the highest rate in 12 years.
In it’s most recent study, Quest Diagnostics found that workforce use of illicit drugs across the board—including cocaine, marijuana and methamphetamine—has climbed to the highest rate in 12 years.
Overall positivity in urine drug testing among the combined U.S. workforce in 2016 was 4.2%, a 5% relative increase over last year’s rate of 4%—the highest annual positivity rate since 2004 (4.
5%), according to an analysis of more than 10 million workforce drug test results.