Opioid abuse continues to be a serious public health problem, one that spills into the workplace far too frequently via workers compensation insurance claims.
Two recent studies from the Workers’ Compensation Research Institute (WCRI) help business executives and policymakers understand how physicians in a workers comp setting prescribe and monitor the use of this frequently abused class of drugs.
The first study shows how frequently physicians performed recommended follow-ups that reduce the chance for opioid abuse. The vast majority of longer-term opioid users don’t receive recommended testing for cases like theirs.
The second study shows that physicians in two states–Louisiana and New York–prescribed opioids at a far higher rate than is the norm elsewhere.
It has been more than two years since the federal Centers for Disease Control and Prevention (CDC) declared an epidemic of prescription painkiller abuse. Overdoses from prescription painkillers like hydrocodone (Vicodin), methadone, oxycodone (OxyContin) and oxymorphone (Opana) kill more people than heroin and cocaine combined, according to the CDC.
The first study, Longer-Term Use of Opioids 2nd Edition, looked at the prevalence of longer-term use of opioids in 25 states from 2010 to 2012 and was a follow-up to similar work stretching from 2008 to 2010. It examined how often the services recommended by medical treatment guidelines were used for monitoring and managing chronic opioid therapy. Those services include drug testing and psychological evaluations and treatment, which may help prevent opioid misuse resulting in addiction and even overdose deaths.
The study found a sizable increase across states in the use of drug testing over the study period, compared with the prior study. In some states, however, the percentage of longer-term opioid users who received these services was still low.
In the typical state, drug testing was used in 25% of all claims involving longer-term opioid use. That’s a larger percentage than found in the earlier study, in which 16% of claims included drug testing in the typical state. On the other hand, it means that in the median state, 75% failed to receive a recommended treatment guideline that would help battle a national drug-abuse epidemic.
While psychological evaluations are also recommended as part of monitoring patients receiving opioids, they were rarely performed: 10% of the time or less in most states. The 25 state median was 5%, basically unchanged from the prior study.
This means that in a typical state, 95% of patients failed to receive a treatment recommended to minimize the chance that an injured worker will sink into drug addiction.
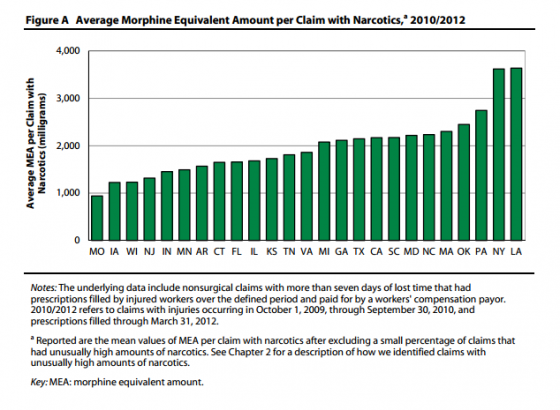
The second WCRI study found striking levels of narcotic use among injured workers in New York and Louisiana. The study, Interstate Variations in Use of Narcotics 2nd Edition, examined trends in the use of narcotics and prescribing patterns of pain medications in the workers’ compensation system across 25 states.
According to the study, the average injured worker in New York and Louisiana received more than 3,600 milligrams of morphine-equivalent narcotics per claim, twice as much as in the typical state.
That amount is equivalent to an injured worker taking a 5-milligram Vicodin tablet every four hours for four months, or a 120-milligram morphine-equivalent daily dose for an entire month—a striking figure.
Throughout the country, the prescription of narcotics for pain relief is prevalent. In the study period, between 65% and 85% of injured workers who received pain medications got narcotics.
The danger of narcotic misuse resulting in death and addiction constitutes a top-priority public health problem in the United States. Employers are concerned as well; they want their workers to recover from injuries and, not incidentally, they desire to keep workers compensation costs reasonable.
Employers can educate injured workers about the dangers of opioids. Workers don’t want their lives torn apart by drug abuse, and no employer would want them to suffer. Employers also reduce their workers compensation costs by avoiding unnecessary opioid use.